|
Congenital Sucrase-Isomaltase
Deficiency (CSID) Society 501c3 Pending |
|||||||
|
Articles What is CSID? Diagnosing CSID Medical Resources Symptoms Typical Emergencies Hospital Visits Sucrose Free Drugs Doctors & Dieticians Medical Alert Tags Support Contact Us Nutrition Food Composition Charts Recipes Induction Diet Cracker Test MedDiary Holidays Resources & Supplies Treatments Sucraid™ Enzymes Vitamins Vaccinations Research Genetic Information Colon Cancer CSID Research Reading Room Journal Articles Slide Decks FAQ School Forms Children's Corner Family Experiences |
Symptoms
We currently track over 12,000 children and
adults with CSID, and we also track approximently 60,000 carriers (parents, siblings, aunts & uncles,
cousins and grandparents
and other extended family members) who carry the disorder.
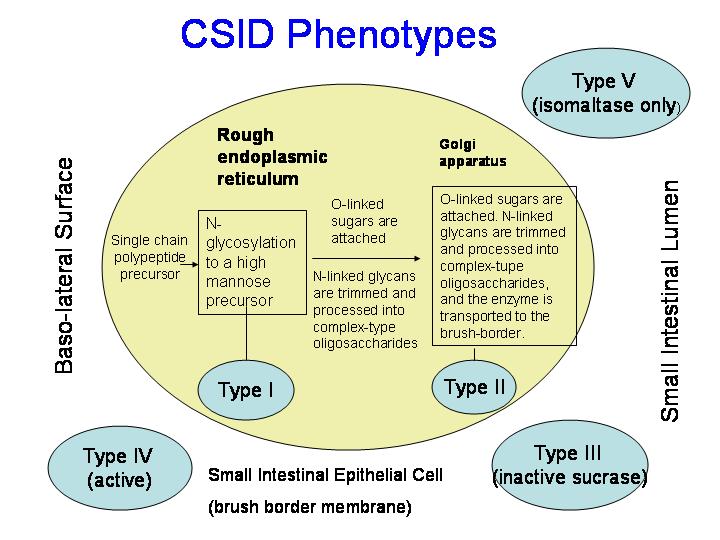
Phenotype
A
52% Sucrose (<2grams) and Starch, some are also Lactose Intollerant Phenotype B 7% Sucrose (<2 grams), Limited Starch, some are also Lactose Intollerant This group cannot ingest sucrose but can ingest limited amounts of starch without becoming symptomatic, usually with chronic watery and or acidic diarrhea, abdominal pain, gas. This group is usually given Sucraid to aid in sucrose digestion of naturally occurring sucrose in fruits and vegetables and an occasional special occasion. Starch is given in limited amounts. Patients in this group must determine the number of grams of naturally occurring sucrose tolerated by the body with one and two mil. dosing of Sucraid. We have very little record keeping of the maximum amount of sucrose that can be tolerated with Sucraid for this group what limited information we do have suggests up to 16 grams per 100 grams of food per meal. This varies quite a bit between children. Doctors may wish to determine the amount of sucrose and starch consumption possible by the child by adding one gram of starch or sucrose that naturally occurs in grains, fruits or vegetables every other day until max. load in any given meal and day is determined. One study should be done for starch and another for sucrose tolerance while using Sucraid after the child has reached a normal body weight and has been symptom free for 21 days. Physicians may consider testing children twice once at one year and again at 3-1/2 as children in this group seem to improve in starch digestion between that period. Contrary to published research the society has not been able to document improvement in starch digestion after 3-1/2 years of age and have not documented any improvement in sucrose digestion at any age for this group of mutations. Children have a load problem for meals as well as an accumulation during the day. Consultation with a dietician is advised. Children under the age of two usually receive daily vitamin supplementation from formula. Children over the age of 2 usually require vitamin supplementation in a sucrose and starch free base. Phenotype C 38% Sucrose (<2 grams), Near Normal Starch, Few are Lactose Intollerant This group cannot ingest sucrose but can ingest normal amounts of starch without becoming symptomatic. This group seems to have the most severe symptoms, chronic watery and or acidic diarrhea, blood in the stool, vomiting, dehydration. Small children two and under and infants can loose as much as 20% of their body weight in 4 to 72 hours when sucrose is first introduced to the diet or with accidental ingestion, some have irregular heart rates as well. This group is usually given Sucraid to aid in sucrose digestion of naturally occurring sucrose in fruits and vegetables and an occasional special occasion. Starch is given in normal amounts after the age of three. Patients in this group must determine the number of grams of naturally occurring sucrose tolerated by the body with one and two mil. dosing of Sucraid. We have very little record keeping of the maximum amount of sucrose that can be tolerated with Sucraid for this group what limited information we do have suggests between 12 and 40 grams per 100 grams of food per meal. This varies quite a bit between children based on their specific mutation. Doctors may wish to determine the amount of sucrose and starch consumption possible by the child by adding one gram of starch or sucrose that naturally occurs in grains, fruits or vegetables every other day until max. load in any given meal and day is determined. One study should be done for starch and another for sucrose tolerance while using Sucraid after the child has reached a normal body weight and has been symptom free for 21 days. Physicians may consider testing children twice once at one year and again at 3-1/2 as children in this group seem to improve to an almost normal level of starch digestion between that period. Some children in this group consume a normal amount of starch twice a day, the third meal seems to exceed tolerance levels and gas and loose stools occur. We have been able to document a temporary improvement in sucrose digestion between ages 11 and 27, with symptoms reoccurring in mid to late adulthood without Sucraid. We have also documented a statistically significant increase in colon cancer and other bowel disorders in CSID patients, parents, grand parents and extended family members with this mutation who were not diagnosed as a child and did not receive Sucraid to aid in sucrose digestion during childhood or who were diagnosed as an infant or child but continued to eat sucrose and starch in normal amounts without sucriad. Children have a load problem for meals as well as an accumulation during the day. Consultation with a dietician is advised. Children under the age of two usually receive daily vitamin supplementation from formula. Children over the age of 2 usually require vitamin supplementation in a sucrose and starch free base. Phenotype D 2% Sucrose (<2 grams), Starch and Lactose Intollerant This group is usually found in Australia and New Zealand and cannot ingest sucrose, lactose or starch without becoming symptomatic, usually with chronic watery and or acidic diarrhea, abdominal pain, gas, swelling, severe red rashes, and bloating. Some children in this group are also diagnosed with ADHD, ADD, learning disorders, restlessness, and anxiety disorders. Diets which work for groups A, B and C do not seem to work for children in this group. Parents from these countries have contributed to a group D list of foods which most of their children have been able to tolerate. This group is usually given Sucraid to aid in sucrose digestion of less than 1 gram per 100 grams of food containing naturally occurring sucrose in fruits and vegetables and an occasional special occasion. All starch is removed from the diet so ketosis and weight loss can be a problem. Lactose is removed from the diet unless lactase is utilized by the physician. Patients in this group must determine the number of grams of naturally occurring sucrose tolerated by the body with one and two mil. dosing of Sucraid. This varies quite a bit between children. Doctors may wish to consider adding foods with less than one gram of naturally occurring sucrose in fruits and vegetables every other day until max. load in any given meal and day is determined before the age of three. Children have a load problem for meals as well as an accumulation during the day. Doctors may also wish to consider the use of lactase for lactose digestion. Consultation with a dietician is advised. Children under the age of two usually receive daily vitamin supplementation from formula. Children over the age of 2 usually require vitamin supplementation in a sucrose, starch and lactose free base - liquid vitamins may need to be considered where tablets are not available. We have only one family in this group who has multiple family members who have died of colon cancer. Group E -- Recessive Carriers all Mutations Siblings, parents, grandparents, some aunts and uncles and 1st cousins of individuals diagnosed with CSID who are heterozygotes have intermediate enzyme values, mild symptoms in infancy, occasional gas, sudden onset of abdominal cramping and pain, and occasional sudden onset of diarrhea in childhood. In adulthood most siblings and parents and grandparents exhibit no symptoms but 32% suffer from with symptoms ranging from occasional gas and abdominal cramping, to irritable bowel syndrome and colitis. Most parents report that siblings are not big "sweet eaters" and gas usually follows a day when the child has ingested starch in large amounts at all three meals. Of the 32% who have reported symptoms parents and grandparents have reported complete relief of the symptoms usually associated with irritable bowel syndrome and colitis once they reduce their sucrose intake to less than 2 grams of naturally occurring sucrose per 100 grams of food (without Sucraid) and reduce but not eliminate their overall intake of starch. Nearly all who follow the diet for their child's mutation become totally symptom free. Phenotype F < 1%-- Sucrose (< 1 gram), Starch and some are Lactose Intollerant This group cannot ingest sucrose or starch without becoming symptomatic, usually with chronic watery and or acidic diarrhea, abdominal pain, gas. Ths group is extreemly sensitive to sucrose ingestion. This group is usually given Sucraid or other enzyme supplementation to aid in sucrose digestion of naturally occurring sucrose in fruits and vegetables and an occasional special occasion where sucrose exceeds 1 grams per 100 grams of food. Without Sucraid all sucrose is removed from the diet and children adhere to a diet of less than 1 gram per 100 grams of food. All other information is the same as phenotype A. Summary of Symptoms Other symptoms this child and or other children in the research literature present with are:
Common Misdiagnosis Allergic
gastroenteropathy
© CSIDINFO.Com, CSID Society (1994-2016) |